Emphysema has a pathological definition, which is a condition where there is permanent destructive enlargement of of the
airspaces distal to the terminal bronchioles without obvious fibrosis (fig.2). Chronic bronchitis is defined clinically by
the presence of chronic bronchial secretions, enough to cause expectoration, occurring on most days for a minimum of 3 months
of the year for 2 consecutive years. The pathological basis of chronic bronchitis is mucus hypersecretion secondary to hypertrophy
of the glandular elements of the bronchial mucosa. Patients with COPD have features of both conditions, although one may be
more prominent than the other.
The causes of COPD and who is at risk?
Smoking and Bronchial Hyperreactivity
Chronic Bronchitis only really became recognised as a distinct disease rather than a set of symptoms in the late 1950's.
The great British Smogs of the 1950's precipitated the deaths of many patients from respiratory failure, and on the continent,
chronic bronchitis was referred to as the English Disease. There can be little doubt now that the most important risk
factor in the development of COPD is cigarette smoking. The effects of cigarette smoke on the lung are manifold. Cigarette
smoke has been found to attract inflammatory cells into the lungs and stimulates the release of of the proteolytic enzyme
elastase from these cells. Elastase breaks down elastin, a normal structural component of lung tissue, but normally, the lung
is protected from the destructive effect of elastase by an inhibitor, alpha-1 antitrypsin (AAT). However, cigarette smoke
attracts more cells and stimulates the release of more elastase than can be inhibited by the circulating levels of AAT. In
addition, cigarette smoke itself may inactivate AAT therefore swinging the balance in favour of more lung destruction by elastase.
The development of COPD , and in particular emphysema, is thought to be due to the imbalance between the destructive elastase
and protective AAT.
Not all people who smoke, however, develop COPD; and not all patients with COPD are smokers or have smoked in the past.
There seems to be a varying susceptibility to lung damage due to cigarette smoke within the general population. Only a proportion
of smokers (maybe only 10-15%) show a rate of decline of lung function over the years that is fast enough to result in the
severe impairment that is typical of patients who present with breathlessness due to COPD. Susceptible subjects have an accelerated
rate of decline of lung function (50-90ml of FEV1/yr compared with 20-30ml of FEV1/yr after the age of 30 in non-smokers).
Subjects with COPD who stop smoking slow down the progression of disease and may return to normal levels of FEV1 decline.
Unfortunately, they do not improve after they stop smoking (fig 3). By the time subjects are symptomatic with breathlessness,
they will have already have severe impairment of lung function, and stopping smoking at this stage may extend their life expectancy
but may not improve their symptoms.
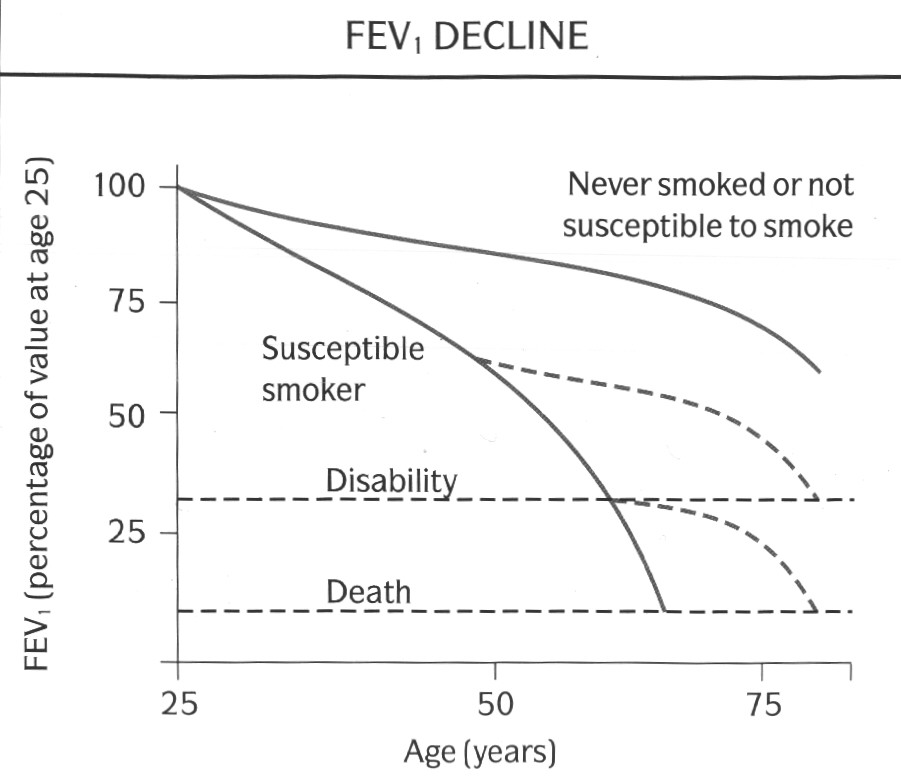
(Fig. 3: graph of survival from Fletcher C, Peto R, Br Med J, 1:1645-1648,
1977, Reproduced with permission)
One possibility to account for these differences is that there is a genetically determined predisposition to develop allergy
and bronchial hyperresponsiveness, the "Dutch Hypothesis". According to this, asthma, emphysema and chronic bronchitis
are different manifestations of a single disease process. Whether an individual develops asthma, bronchitis or emphysema is
a result of genetic and environmental factors that are modulated by age and gender. An alternative school of thought is the
"Two-type Hypothesis", which includes a Dutch-type limb termed "Chronic Asthmatic Bronchitis" or "Overlap
Syndrome", and a more insidious form which leads to "Chronic Obstructive Bronchitis and Emphysema". Both schools
of thought, however, emphasise the inter-relationship between bronchial hyperreactivity (atopy), infection and smoking (fig.4).
Focus has recently been placed in trying to identify the population most at risk of developing COPD.
Fig. 4 : Venn diagram of overlap between asthma, chronic bronchitis and emphysema
(the
diagram is not proportional)
Alpha-1 Antitrypsin Deficiency
Another well established risk factor is deficiency of the protective protease inhibitor, Alpha-1 Antitrypsin (AAT). This
is an inherited autosomal recessive (designated PiZZ) disorder which is fairly rare in the general gene pool. The estimated
prevalence of the heterozygote phenotype (PiMZ) is about 2-3% of the western population. The incidence of homozygous births
is in the region of 1 in 3000 live births. As such, AAT deficiency account for probably less than 5% of all cases of COPD.
Low levels of AAT allow the uninhibited action of elastase on the lung parenchyma giving rise to destruction of the alveoli
and the eventual development of emphysema rather than chronic bronchitis. The pattern of emphysema in AAT deficiency differs
slightly from that of smoking induced pure emphysema in that AAT deficiency produces panlobular emphysema affecting predominantly
the lower lung fields, and smoking induced emphysema is usually centrilobular affecting the upper lung fields initially. Not
all people with PiZZ have very low levels of AAT. Only serum levels below 35% normal are at risk of developing emphysema.
Subjects who are PiMZ may also have reduced levels but not as low as PiZZ, and are not thought to be at more risk from developing
emphysema than PiMM subjects. Subjects who are PiZZ may not progress to have emphysema, but PiZZ subjects who smoke have a
greatly increased risk of developing emphysema, especially at an early age (Fig 5).
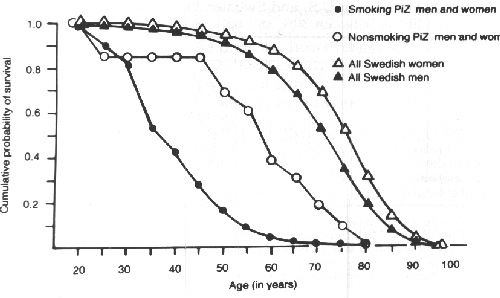
(Fig. 5: Graph of cumulative survival from Larsson C. Acta Med. Scand. 204:345-351,
1978, reproduced with permission)
Air Pollution and Occupational Exposure
The role of outdoor air pollution in the evolution of COPD is still controversial. Respiratory deaths in the UK reached
a peak during the great smogs of the 1950's. Following the passing of the Clean Air Acts of 1956 and 1968 which established
"smokeless zones" in populated areas and allowing only the use of smokeless fuels, the quality of British air has improved.
The people that died during the smogs were people at the greatest risk, i.e. the elderly and infirmed, and those with chronic
respiratory and cardiac problems. The question of whether atmospheric pollution itself can cause or contribute to the development
of COPD is still uncertain.
Outdoor air pollution is very heterogeneous and is different in different areas. It is mainly comprised of particulates
and gases with some background radioactivity. The particulates mainly originate from the incomplete combustion of solid fuels
and diesel, ash and fine dusts. The main gaseous components are the various oxides of sulphur, nitrogen and carbon, again
from the combustion of fossil fuels; hydrocarbons and ozone. Studies from the UK have shown a relationship between levels
of atmospheric pollution and respiratory problems (particularly cough and sputum production) in both adults and children,
and similar studies from the USA have confirmed these findings. Some studies have reported lower levels of lung function in
adults living in highly polluted areas and this seems to related to pollution by acidic gases and particulates. As with the
problem of smoking, there will be individuals who are more susceptible to the effects of atmospheric pollution than others.
Any occupation in which the local environment is polluted with the aforementioned gases and particulates increases the
risk of developing of COPD. In addition, there is evidence that cadmium and silica also increase the risk of COPD. This is
especially true if the subject smokes. Occupations at risk include coal miners, construction workers who handle cement, metal
workers, grain handlers, cotton workers and workers in paper mills. However, the effect of smoking far outweighs any influences
from the work environment.
Passive Smoking
Most of the tobacco smoke in a room it that which is coming form the burning end of the cigarette rather than the smoke
exhaled from the smoker's lungs. This smoke (called sidestream smoke) is actually higher in concentration of toxic
substances than exhaled smoke (mainstream smoke). However, it has been very difficult to judge how much smoke is passively
inhaled and what effects this passively inhaled smoke has on the lungs. Studies on passive smoking are plagued by methodological
difficulties. Studies in which questionnaires are used to assess the degree of passive exposure to cigarette smoke are prone
to bias. Recently, it has been possible to assess the degree of exposure by measuring levels of the nicotine metabolite, cotinine,
either in the blood, saliva or urine. Most of the studies using these techniques have been cross sectional ones on children
from smoking or non-smoking families. The evidence suggests that respiratory infections and respiratory symptoms are more
common in children in households where one or both parents smoke. Also, there is a small but significant difference in the
prevalence of respiratory symptoms and lung function in adults and children who are regularly exposed to passive smoking.
Whether these differences are clinically significant is yet to be resolved.
Infections
The role of viral infections of upper and lower respiratory tract in the pathogenesis of COPD remains to be clarified.
Viral infections in the lung enhance inflammation and predispose to bronchial hyperreactivity. There is increasing evidence
between early childhood infections and increase in respiratory symptoms and lower lung function in adulthood. The viruses
that have been implicated are adenovirus and respiratory syncytial virus. Once COPD is established, repeated infective exacerbations
of airflow obstruction, either viral or bacterial, may speed up the decline in lung function.
Race, Gender and Socioeconomic status
Chinese and Afro-Caribbean races seem to have a reduced susceptibility to developing COPD. It is frequently stated that
COPD is more prevalent in men. However, when smoking and occupational exposure is taken into account, the relative risk of
developing COPD is not significantly higher in men than women. With smoking on the increase in women, it is possible that
women may catch up with men in terms of absolute numbers. The beneficial effects of stopping smoking on the rate of lung function
decline may greater for women than men.
In studies conducted in the UK in the 1950's and 1960's, there is a clear social class gradient for COPD with it being
more prevalent in the lower socioeconomic strata. This may be related to poorer housing and nutrition and use of fossil fuels
for heating without adequate ventilation. Also, there is a higher prevalence of smoking in the lower socioeconomic strata,
and they are more likely to be employed in jobs where they may be a risk from occupational exposure. However, this socioeconomic
gradient fro COPD is now becoming more smoothed out as standards of living improve.
Diagnosis of COPD
History
Most patients will have been smoking cigarettes for many years (probably in excess of 20 pack years). The two main symptoms
of COPD are breathlessness and cough which may or may not be productive of purulent sputum. A history of persistent productive
cough or recurrent infections especially in the winter months is common. The cough is usually worse in the mornings but bears
no relationship to the severity of the disease. Excessive sputum volumes are unusual and may suggest bronchiectasis. Haemoptysis
should alert the physician for the presence of a carcinoma of the bronchus as this is a frequent co-morbidity in patients
with COPD, but is often just due to infective exacerbations
Breathlessness is a common feature of acute infective exacerbations, but breathlessness during normal every day activity
develops insidiously over many years and most patients will have lost more than 50% of their predicted FEV1 by the time that
breathlessness becomes a problem. Wheeze is often an accompanying feature of breathlessness and may be erroneously attributed
to asthma.
Weight loss is common in patients with long standing disease with predominately emphysema (the old fashioned pink puffer),
although weight gain may also be a feature suggesting chronic hypoxaemia and the onset of cor pulmonale (the blue bloater).
Patients can rarely be classified as pink puffers or blue bloaters, and the two states do not have any pathophysiological
correlation. Therefore the usefulness of this classification is questionable and its use is discouraged by both sets of guidelines.
Examination
There are no specific findings on examination, although signs of hyperinflation of the chest are highly suggestive of emphysema.
These include a barrel shaped chest (increased antero-posterior diameter), use of accessory muscles of respiration, reduction
of the cricosternal distance, tracheal tug, paradoxical indrawing of the lower ribs on inspiration (Hoover's sign), intercostal
recession, hollowing out of the supraclavicular fossae, pursed lip breathing and reduced expansion. In addition the patient
may have hyperresonant lung fields, prolongation of expiration, especially forced expiration >5s, and audible wheeze. None
of these signs are specific to COPD and do not correlate very well with the severity of the disease which emphasises the need
for objective assessment. Their presence, however, should alert the physician to the possible diagnosis of COPD.
As the disease progresses, signs of right ventricular dysfunction may develop (Cor pulmonale) because of the effects chronic
hypoxaemia and hypercapnia which include peripheral oedema, raised jugular venous pressure, hepatic congestion, and the presence
of metabolic flapping tremor. Despite the widely held belief that these signs are due to right ventricular failure, the pathophysiology
cor pulmonale is likely to be due to altered renal function giving rise to salt and water retention rather than cardiac dysfunction
secondary to pulmonary hypertension.
Measurements of Lung Function
Both sets of guidelines emphasise the use of simple spirometric measurements to assess the severity and predict the prognosis
of patients with COPD. However, they are less specific on the use of the other measurements of lung function in the diagnosis
and management of COPD. It is probably good practice to perform routinely a minimum of spirometry with bronchodilator reversibility,
static lung volumes, carbon monoxide gas transfer and pulse oximetry as baseline measurements. The addition of walk distance
and a quality of life questionnaire may also be helpful as a baseline for future reference
1. Spirometry
In the European guidelines, the presence of mild airflow limitation is recognised by a reduction in the ratio of FEV1 to
VC or FVC (<1.64 residual standard deviation below predicted FEV1/VC). In both sets of guidelines, severity is based on
the measured FEV1 as a percent of predicted FEV1. The European guidelines define 3 stages of severity:
| 1. FEV1>=70% predicted : Mild |
| 2. FEV1=50-69% predicted : Moderate |
| 3. FEV1<50% predicted : Severe |
The American guidelines however stage the severity of COPD as:
| 1. FEV1>=50% predicted : Stage I |
| 2. FEV1=35-49% predicted : Stage II |
| 3. FEV1<35% predicted : Stage III |
Therefore a subject in the European Severe category may only be the equivalent of American stage II, and there is no European
equivalent for the American stage III. This may lead to problems in the future when trying to compare trials in the managment
of COPD patients. There is likely to be few patients recognised in the mild to moderate European stages since many of these
patients will not be very symptomatic and will remain undiagnosed unless specifically screened for.
Most modern electronic spirometers will be able to produce an expiratory flow-volume curve or loop. The appearance of the
flow volume curve is highly characteristic is airflow obstruction, especially when there is dynamic airways compression as
in patients with predominately emphysema (fig 4). The flow volume loop in severe airflow obstruction is a good graphical representation
of the severe impairment of airflow at low lung volumes due to dynamic airways compression. This information can also be obtained
as absolute values from the spirometer. Neither set of guidelines emphasises the utility of flow volume loops as an aid to
diagnosis although the appearances in severe disease are fairly specific. Severely obstructed flow volume loops may also be
seen in obliterative bonchiolitis although there should be little difficulty in differentiating between the two on history
alone.
Fig. 6: Flow volume loops showing normal and severe airflow obstruction
The absolute value of the FEV1 and the yearly rate of decline of the FEV1 may also provide information on the prognosis.
The FEV1 at diagnosis can be a predictor of long term survival (fig 7). The yearly loss of FEV1 is about 20-30ml/yr after
the age of 30 in normal non-smoking individuals. In smokers susceptible to developing COPD, the rate may increase to 50-90ml/yr
(link to "Smoking and Bronchial Hyperreactivity) and fig 2) and thus this susceptible population can be identified and efforts
increased to stop them smoking before developing disabling disease.
Fig. 7: Graph from Anthonisen NR et al, Am Rev Respir Dis 1986; 133:14-20
The use of peak expiratory flow rate (PEFR) for diagnosis is not recommended but may be useful for domiciliary monitoring
or to document diurnal variation to differentiate from asthma. However, in severe COPD, the PEFR will tend to seriously underestimate
the severity of airflow obstruction.
2. Response to bronchodilators and corticosteroids
Most patients with COPD will show an increase in FEV1 in response to a bronchodilator, and some by more than 15% of the
baseline value (which is often used as a diagnostic test for asthma), but never back to normal levels of lung function. In
COPD. expressing reversibility as a percentage of baseline values is of limited value because of its dependence on the pretreatment
level. Expression of reversibility as an absolute value or as a percentage of predicted values is more reproducible and independent
of baseline FEV1. Improvement of the peak flow in response to bronchodilator is not recommended as a guide to reversibility.
Many patients report subjective symptomatic improvement without any objective change in their spirometry. The absence of measurable
spirometric reversibility therefore is not a reason to withhold bronchodilator treatment.
Some patients with stable COPD may show an increase in FEV1 following a prolonged trial of oral corticosteroids (e.g. Prednisolone
40mg od for 2 weeks). In Europe, this is often seen as an indication for continuing these drugs long term via the inhaled
route. However, routine spirometry may not identify all responders to oral corticosteroids, since the improvement may be due
to a reduction in FRC and an increase in FVC rather than FEV1. Therefore, there is case for measuring full lung function at
the beginning and end of a trial of oral corticosteroids.
3. Static lung volumes and lung compliance
Total lung capacity (TLC), residual volume (RV) and functional residual capacity (FRC) are all characteristically increased
in COPD and are related to the degree of hyperinflation of the lungs, especially when there is predominately emphysema. Although
these measurements are useful and can help differentiate COPD from asthma, neither set of guidelines suggests that the use
of these tests is essential in the diagnosis and managment of COPD. Similarly, although lung compliance is increased and lung
recoil pressure is reduced and there are characteristic changes in the pressure-volume curve, these measurements are mainly
research tools and not necessary in routine clinical practice.
4. Gas Transfer
Carbon monoxide gas transfer capacity (DLco)and coefficient (Kco) are both reduced in symptomatic patients with COPD. The
transfer coefficient is a good indicator of the presence and severity of emphysema and thus reduction in the Kco is helpful
in distinguishing patients with emphysema from those with asthma. There are also studies which relate the likelihood of hypoxaemia
at rest and on exertion to the level of the Kco.
5. Pulse Oximetry and Arterial Blood Gases
The relationship between symptoms, FEV1 and hypoxaemia is weak. The combination of FEV1 and gas transfer strengthens the
prediction of resting hypoxaemia. Regular assessment of hypoxaemia is recommended in all patients with moderate to severe
COPD (hypoxaemia is more likely when FEV1<1.0l). Rather than regular arterial blood gases analysis, it would be more sensible
to use pulse oximetry as a screening test since this is a simple, cheap, painless and non-invasive technique which is fairly
accurate. A reasonable strategy would be to perform pulse oximetry on all patients and perform arterial blood gas analysis
only on patients with an arterial saturation of less than 93% (since this equates to PaO2 of about 8kPa or 60mmHg on the haemoglobin-oxygen
saturation curve). Arterial blood gases should always be measured in patients with suspected CO2 retention. although this
will rarely be present in the absence of arterial hypoxaemia and desaturation.
Imaging
1. Chest X-ray
The presence emphysema can be suspected on routine chest radiography but this is not a sensitive technique for diagnosis.
Large volume lungs with a narrow mediastinum and flat diaphragms are the typical appearances of emphysema Fig.8). In addition,
the presence of bullae and irregular distribution of the lung vasculature may be present. In more advanced disease, the presence
of pulmonary hypertension may be suspected by the prominence of hilar vasculature. The chest X-ray is not a very good indicator
of the severity of disease and will not be able to identify patients with COPD without significant emphysema. However, the
chest X-ray is useful to look for complications during acute exacerbations and to exclude other pathology such as lung cancer.
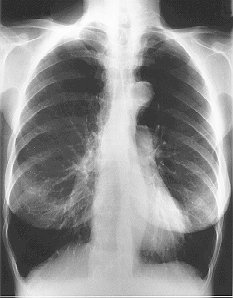
Fig. 8: Typical CXR of emphysema
2. CT scan
Computerised tomography of the chest, especially with an high resolution algorithm (HRCT) has much greater sensitivity
and specificity than plain chest radiography in diagnosing and assessing the severity of emphysema (fig 9). CT can identify
areas of bullous disease that may be amenable to surgery that is not evident on plain chest radiography and is useful in predicting
the outcome of surgery. HRCT is also capable of differentiating between the various pathological types of emphysema. However,
the use of CT scanning in the routine clinical assessment of patients with COPD is not recommended by either set of guidelines,
and is reserved for patients in which the diagnosis is in doubt, to look for co-existent pathologies and to assess the suitability
of surgical intervention.
(Fig. 9: HRCT of emphysema)
Other tests
1. Exercise testing
The routine assessment of functional capacity is not recommended in either set of guidelines. This is rather surprising
since often the main presenting symptom is limitation of walking and other activities of daily life by breathlessness. Since
FEV1 and other measurements of lung function are poorly correlated to function capacity and subjective sensations of breathlessness,
an objective measurement of the main presenting problem should be useful in helping to determine therapies that are actually
beneficial. There may be little point in prescribing a treatment that may improve airflow obstruction, but the patient gain
any improvement in functionality. Currently, the physician relies heavily on the the subjective sensations of the COPD patient
to help determine the efficacy of therapy. Thus, there may be a case for the routine assessment of of functional capacity
with simple tests such as six minute walk distance or shuttle walk distance in the managment of patients with moderate to
severe COPD. The European guidelines states that the reproducibility of these tests is poor, yet they are frequently used
as research tools in the development of new treatments for COPD. The use of more sophisticated tests of exercise performance
such as VO2max should be limited to research or when the diagnosis is in doubt (i.e. when breathlessness is out of proportion
to the degree of impairment of lung function).
2. Quality of Life
There are several established questionnaires on quality of life (QoL) in chronic respiratory disease available (e.g. St.George's
Hospital Respiratory Questionnaire, Chronic Respiratory Questionnaire) and other general health questionnaires with a respiratory
component (e.g. SF-36, Nottingham Health Profile). Also, there are questionnaires on anxiety and depression which can contribute
significantly to symptoms in COPD (Hospital Anxiety and Depression Score). These tools are frequently used in studies on the
efficacy of new treatments in COPD but none have been accepted for use in everyday practice and have not been recommended
for routine use. However, quality of life considerations are becoming increasingly important, and soon measures of QoL will
soon be essential.
3. Sleep Studies
Many patients with COPD may have worsening hypoxaemia and hypercapnia during rapid eye movement (REM) sleep, and if this
is combined with obstructive sleep apnoea it is called the Overlap syndrome. The role of nocturnal desaturation in the evolution
of pulmonary hypertension is uncertain. Those who are most likely to desaturate at night are those who are already hypoxaemic
during the day. Detailed sleep studies are currently only recommended in those with additional suspected obstructive sleep
apnoea or those with cor pulmonale or polycythaemia with only mild or moderate COPD.
Forthcoming sections (so visit regularly)
Mucolytic agents
Oxygen and Long term oxygen therapy
Antibiotics
Prevention of infection
Pulmonary Rehabilitation
Treatment of acute infective exacerbations
Non-invasive assisted ventilation in management acute hypercapnic respiratory failure secondary to COPD
Lung Volume Reduction Surgery
The British Thoracic Society COPD Guidelines

